* By Dr. Johan Svenson
Millions of people suffer from the devastating effects of opioid addiction, so finding alternative ways to manage pain is a global priority. It may seem unlikely, but a toxic microalgae — a former villain, now potential hero — could help reduce our reliance on opioids in the future. Below I explain how farming a specific microalgae through aquaculture could produce a powerful, non-addictive painkiller.
Millions of people suffer from the devastating effects of opioid addiction, so finding alternative nage pain is a global priority. It may seem unlikely, but a toxic microalgae — a former villain, now potential hero — could help reduce our reliance on opioids in the future.
Below I explain how farming a specific microalgae through aquaculture could produce a powerful, non-addictive painkiller.
Aquaculture of finfish, shellfish, macroalgae, and emerging low-trophic species is a growing global industry, offering sustainable, low-carbon food sources. Microalgae aquaculture is gaining attention as a land-based source of proteins and lipids, but its development is still constrained by high production costs and technical challenges associated with scaled production. As a result, global microalgae production remains relatively small.
Microalgae and cyanobacteria (photosynthetic bacteria) are fascinating organisms that sit at the base of the marine food web, using sunlight to generate both nutrition and oxygen — a vital function for life on Earth. However, under certain environmental conditions, some species of freshwater and marine microalgae produce harmful algal toxins during what are known as harmful algal blooms (HABs). These toxins vary in form, and some — such as ciguatoxins, saxitoxin, and microcystins — are among the most potent known to science.
Shellfish, which are filter feeders, can accumulate these toxins. When consumed by humans through contaminated seafood or water, they can cause serious illness or even death.
Fortunately, scientists closely monitor these species, and any microalgae grown for consumption are rigorously screened to ensure they are safe and non-toxic.
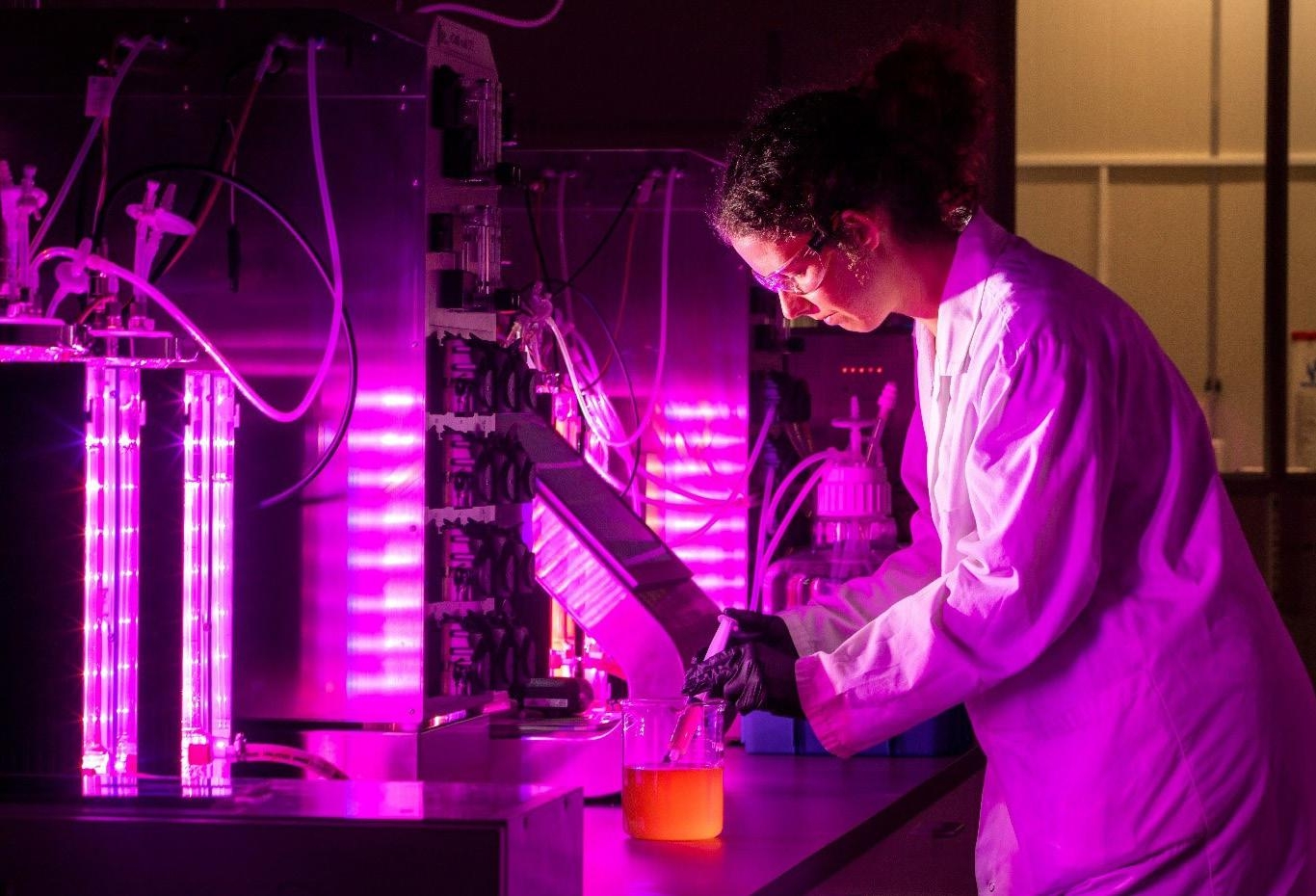
With that in mind, it may seem surprising that a team of scientists at Cawthron Institute in New Zealand is actively scaling up aquaculture of one of these toxic species in large, shiny photobioreactors. The team is farming Alexandrium pacificum, a dinoflagellate commonly linked with HAB events in the South Pacific and responsible for many cases of seafood related poisoning. Ingesting this algae would be dangerous — luckily, that’s not the purpose of the farming. Cawthron scientists, who have spent decades studying HABs, are well aware of the toxic cocktail this algae can produce. In fact, those very toxins are the reason they’ve chosen to grow it at scale.
To understand why, we need to take a step back and explore the world of drug discovery. Simplified, modern medicine is based on synthetic compounds and bioactive compounds from nature with an ability to cure or prevent diseases. Initially, all drugs were derived from natural products and these compounds still play a big role, despite the development of modern synthetic chemistry, computational chemistry and AI.
Currently, about one third of all approved drugs are derived from natural compounds and their contributions is even more pronounced in the fields of antibiotics and cancer. Mother Nature is unrivalled in coming up with exciting chemistries and unexpected bioactivities.
Natural toxins and venoms are produced for defensive purposes or for hunting, and while they are certainly not originally designed to be neither beneficial or helpful, some of them have pharmacological properties that allows them to be used in medicine. Examples include snake venom derived drugs against high blood pressure as well as marine drugs against cancer and pain.

The Opportunity
This brings us to algal toxins. Many of these compounds work by blocking ion channels — protein pores in our cells that regulate essential functions by allowing ions to flow in and out. Block the wrong one, and the results can be fatal: paralysis, loss of breathing, or cardiac arrest. This is how many HAB-related toxins affect the body.
But not all ion channels are created equal, and not all toxins act indiscriminately. Some show a preference for certain channels over others, which opens the door to selective medical use. For example, a toxin might block pain-sensing nerve receptors (nociceptors) without interfering with other vital systems. One such compound is neosaxitoxin — a relative of the potent algal toxin saxitoxin, which is an effective sodium channel blocker.
This discovery — that neosaxitoxin can block pain signals in sensory neurons — sparked interest among scientists from the Chilean company Proteus, Boston Children’s Hospital, and Harvard Medical School. Their early research showed neosaxitoxin was a promising treatment for post-operative pain when used in combination with adrenaline and the approved painkiller bupivacaine: long-lasting, localized, with no systemic side effects, and crucially, non-addictive. This makes it a compelling alternative to opioids.
A single dose of neosaxitoxin, combined with adrenaline and the approved anesthetic bupivacaine, could provide up to 72 hours of pain relief. The compound is so potent that one gram is enough for a staggering 25,000 doses — a remarkable achievement.
The Challenges
So why isn’t this compound being used in drugs already if these initial promising discoveries were made and published almost two decades ago?
There are several reasons. First, any drug must pass through stringent clinical trials to show safety and function. To conduct those trials, you need access to reliable, pure material — something that’s been extremely difficult for neosaxitoxin. While it’s a small molecule, it is chemically complex and has proven difficult to synthesize in useful quantities.
Early trials relied on toxins extracted from contaminated shellfish, but this is not a scalable or reliable method. The complexity of the molecule has also prevented cost-effective production using recombinant or microbial fermentation technologies.
Even more challenging is the fact that algae produce these toxins as part of a chemical cocktail — a mix of compounds so similar it becomes difficult to isolate pure neosaxitoxin. So, is the idea dead in the water?

The Solution: Microalgae Aquaculture
Not quite. This is where Cawthron’s team devised a clever workaround.
Rather than isolate neosaxitoxin directly, they found a way to extract and isolate a more abundant compound — gonyautoxin 1,4 (GTX-1,4) — from the algal mixture and convert it into neosaxitoxin through a single, targeted chemical step. This semisynthetic route made large-scale production theoretically viable, but only if Alexandrium pacificum could be reliably domesticated and grown at scale.
As anyone familiar with aquaculture knows, domesticating a new species is no easy task and toxic marine microalgae are no exceptions. The team began by screening Cawthron’s national microalgae collection to identify a strain that could grow efficiently and produce large quantities of GTX-1,4. This was done at a small scale (200 mL), eventually yielding a strong candidate strain.
With the right strain selected, the next hurdle was scaling up. While some researchers have grown dinoflagellates in lab-scale volumes (litres), few have succeeded at large scale. Strict control over growth conditions is essential for pharmaceutical production, so natural seawater couldn’t be used given the associated natural variability and risk of contamination.
Instead, the team developed a custom artificial seawater solution prepared in-house — no small feat, since dinoflagellates typically dislike artificial media. Growth and toxin yields had to be meticulously optimized to generate a satisfactory yield.
Light and temperature, being key to photosynthesis, also had to be finely tuned. After extensive experimentation, the team succeeded in producing dense cultures with toxin concentrations 30 times higher than in natural algal blooms.
The result? A reliable, scalable process producing 1–1.5 grams of GTX-1,4 from a single 1,250-litre photobioreactor every two weeks.
This perhaps doesn’t sound like much but given that the global demand is estimated at 500–1,000 grams annually, this process could supply both clinical trials and future commercial production. It also shows that aquaculture is about more than fish, mussels, and seaweed — we’re only beginning to unlock its full potential.
Will This Be the Next Paracetamol?
Neosaxitoxin is a highly potent, watersoluble drug lead designed for hospital use only. It must be injected and is co-administered with other compounds, so it won’t replace over-the-counter options — but it could offer a game-changing option for post-surgical pain relief by dramatically reducing the need opioid pain medications. The compound has successfully completed Phase 1 clinical trials.
Now, the Cawthron team and its partners, including AlgavitaBio Inc., a U.S. based biotechnology company, are working to secure funding for Phase 2 — a crucial step toward turning this promising compound into a realworld solution for pain.
* Dr. Johan Svenson, Science Impact Manager, Cawthron Institute E-mail: johan.svenson@cawthron.org.nz